I got COVID-19, and I recovered. Below are the details of my experience and the COVID treatment protocols I used to get better.
Medical Disclaimer: The below does not constitute medical advice. It is presented for informative purposes and to detail my own COVID-19 experience, including what treatments I used. You should discuss COVID-19 treatments with your physician, especially if you have pre-existing conditions.
By Nate Doromal
I want to paint an honest picture of what getting COVID-19 was like. There are cases of people who got it but are largely asymptomatic or have symptoms akin to a cold. In contrast, I got decently sick – overall still considered mild COVID but akin to some of the tougher flu cases I have experienced. It took me a full two weeks until I could say I was recovered, which is pretty typical for mild cases.
While getting COVID-19 was no walk in the park, too often, the media paints too fearful a picture of it, emphasizing dying people on ventilators and then long-haul COVID. The truth is that over one hundred million Americans, including myself, have recovered from COVID-19, and you have the ability to do so too.
With so many people getting COVID -19, the focus of medicine should have been how to treat early COVID effectively at home to minimize the possibility that it will worsen. Here I hope to share knowledge regarding early treatment.
What is it like to get COVID-19?
I believe in the resiliency of the immune system. For a lot of the pandemic, I traveled around the country just fine without getting sick. I took care to do social distancing but generally avoided wearing a mask when I could (the medical rationale for widespread masking is weak). But, after a particularly stressful month of work, I suppose the stress had depressed my immune system enough, such that I got infected by COVID-19.
For two days, I felt like I had a cold coming down. But then, I got full-blown sickness with fever, chills, and body aches. Suspecting COVID, I started parts of the FLCCC Early Outpatient I-Mask+ Protocol that evening. I took a dose of ivermectin, vitamin D3, vitamin C, quercetin, and zinc. I was lucky in that I had prepared all of this in advance just in case I came down with COVID.
The Front Line COVID-19 Critical Care Alliance is a group of front-line clinicians whose purpose is to research and develop effective treatment protocols for COVID-19. They pioneered a hospital treatment protocol for severe cases and the early treatment protocol, which I used. They have extensively researched the efficacy of Ivermectin. Their early protocol is as follows:
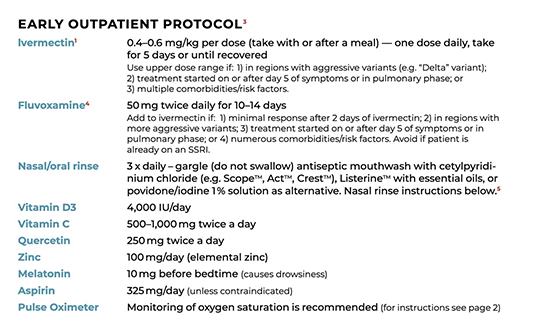
I did not use Fluvoxamine during the time I was sick as I didn’t have it on hand. I did not do the nasal/oral rinse, though, given the mouth problems I later experienced, I wish I had.
I was completely floored during the first three days. I had a moderate fever, chills, and the fatigue was such that I had to lie down in bed all day long. My body ached all over, sufficiently enough that it was difficult sleeping. On top of this, I had a pretty bad headache. Oddly enough, I did not have any cough and sore throat, but I did have some swelling in the salivary glands. I was lucky not to have any shortness of breath during the entire time I was sick.
I drank a lot of fluids (mainly herbal teas with honey). I got a respite from the fever, chills, and body aches by taking hot baths with Epsom salt thrice a day. I had little to no appetite during these first initial days.
A well-meaning friend sent me this COVID case guideline, but the only part I agreed with was the guidance on fluids. There was no way I could have physically consumed 2000 calories and 75-100 grams of protein in my state during those first couple of days. The only things I could eat were soups and bone broth. There is wisdom in the body in suppressing appetite as it only allows the energy that would be used for digestion to be devoted to healing.
My headache picked up on day 2, and in response, I added aspirin and added 10 mg of melatonin in the evening and continued using this for the next five days until the headache got to be tolerable. This helped me with my sleep. However, I am not in the habit of using painkillers, so I limited my aspirin to just one dose of 325 mg at bedtime.
On day 3, my fever and chills continued, and I remained in bed all day long. I started megadosing vitamin C until bowel tolerance, taking around 10-15 grams orally per day. I continued using vitamin C during the remainder of the time I was sick.
On day 4, I felt strong enough to sit at a desk and use a computer. I had a bad spasming headache that lasted all day. My fever broke, and my chills abated. I noted today that my gums had become swollen and painful. Looking at the research, I learned that the mouth tissue has ACE2 receptors, making it a target for the SARS-CoV-2 virus. My appetite had come back somewhat, but due to my mouth condition, eating was painful.
On day 5, I felt a lot stronger. I still had a headache, and I was still sick. But it was more like a normal sick instead of a COVID sick. My improvement was substantial enough to feel confident that I was out of the woods and that I would not get severe COVID.
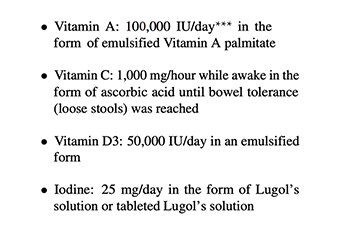
On day 6, I felt about the same as the previous day. I was still sick, and I felt like this virus was hanging around. So I started the Brownstein Protocol, which Dr. David Brownstein developed. He used this protocol to treat over 500 COVID patients with zero deaths and a very low hospitalization rate. The goal of the protocol is to boost the body’s immune system capabilities to fight off the virus.
It consists of the below vitamin oral supplements and the use of a nebulizer with 0.04% hydrogen peroxide with one drop of 5% Lugol’s iodine:
A nebulizer is a medical device that converts liquid medication into a mist so it can be inhaled into the lungs (the one I used is here). While hydrogen peroxide is known as a disinfectant that can kill viruses and bacteria, it is less known that our own white blood cells use hydrogen peroxide as a weapon against infection. At the start of the pandemic, I purchased one after seeing anecdotal reports that it helped against COVID. I used the nebulizer 1-2x times a day.
From days 6-10, I stayed on the Brownstein protocol. I noted that midday, after taking the vitamins, that I felt a boost in my energy. My headache and fatigue were still present, but I saw steady improvement day-to-day. On day 8, I started taking 600 mg of NAC after learning research that suggested it can inactivate the SARS-CoV-2 virus.
My mouth was still giving me problems. My gums were still swollen, and it was surprisingly uncomfortable. I started to treat it actively. Overall though, improvement for my mouth was slow.
I started oil pulling twice a day using coconut oil with two drops of clove essential oil. Clove oil is a known natural remedy for helping with swollen gums, and I got some immediate relief from it. I also started taking 4,000 mg of lysine to promote mouth wound healing. I also started using colloidal silver, purported to have anti-bacterial and anti-viral properties. I would take a teaspoon of it and swish it around my mouth before swallowing it five times per day. The use of the nebulizer also helped my mouth.
On days 11-13, I noticed that my energy levels got better each day, but some fatigue and headache persisted. I pushed down my vitamin intake to 25,000 IUs of Vitamin A, 8,000 IUs of Vitamin D, 50 mg of zinc, and 8 mg of iodine. Mouth started to feel better by day 12 though some minor swelling remained even past day 14.
By day 14, I was feeling good enough that I could say I had recovered. Certainly, it was not yet time to do heavy exercise, but I was back to doing work and chores around the house.
In retrospect, if I had to re-do my treatment protocol, I would have started the FLCCC I-Mask+ protocol and the Brownstein vitamin protocol concurrently. I missed a few days of ivermectin doses because I did not think I needed it anymore. Had I known the COVID would hang on the full two weeks, I would not have missed any doses. I also would have started treating my mouth earlier as soon as I had indications it was a problem. I felt like I also got a lot of benefits from nebulizing so that I would have started immediately.
I had chosen these particular protocols largely due to familiarity since I had been actively researching them. There are other good protocols, including the Zelenko protocol (which makes use of HCQ) and the Bartlett protocol (which makes use of budesonide). Dr. Peter McCullough has a good guide to COVID early treatment (available free here).
I recommend doing research on all of the discussed protocols and then discussing options with your physician. It is better to have your homework done and have a plan before you need it. For example, you should be familiar with obtaining ivermectin (see instructions at FLCCC and at America’s Frontline Doctors). Those sites also list front-line doctors who are experienced in treating COVID-19 and are available for telehealth sessions.
What are the risks from COVID-19?
In reality, there is a wide variety of demographic and genetic profiles in society, and not all of us will be equally affected by COVID-19. Often the media likes to make the risk decision for us while neglecting to tell us the actual probability of harm or that these probabilities differ per person.
An examination of the CDC document “COVID-19 Pandemic Planning Scenarios” (last updated March 19, 2021), the odds of death are as follows:
| 0–17 years old: 20 | 1 in 50,000 |
| 18–49 years old: 500 | 1 in 2,000 |
| 50–64 years old: 6,000 | 1 in 167 |
| 65+ years old: 90,000 | 1 in 11 |
To put these statistics into perspective, the FBI in 2018 calculated the murder rate to be 1 in 20,000. The odds of dying in a motor vehicle crash in 2019 were approximately 1 in 8,400.
Additionally, having one or more pre-existing conditions (also called co-morbidities) affects the risk of severe COVID-19 infection. Some of these conditions include asthma, diabetes, cancer, obesity, having a heart condition, etc.
There are studies to indicate that a nutrient deficiency can serve as a risk factor for severe COVID. For example, this study found that deficiencies in vitamin D or selenium may affect the immune system and increase the risk for severe COVID. Another study identified the importance of essential nutrients zinc, ω-3 polyunsaturated fatty acids (PUFAs), vitamin D, and magnesium for both the prevention and treatment of COVID-19.
Even if one recovers, there is the possibility of long-haul COVID, a condition in which symptoms persist 60 days or more after recovery. According to a University of California study, long-haul COVID occurs in a minority of non-hospitalized patients, roughly 27%. It should be noted that there are options to treat long-haul COVID, such as the FLCCC I-Recover protocol.
Given the above facts, I made the decision that the COVID vaccine was not worth it for me (see my examination of COVID vaccine injury risk). I am 39 years old with no pre-existing conditions and in decent health. I exercise five times a week, and my body weight is in the normal range. I eat a decently good diet with sufficient quantities of organic fruits and vegetables. Based on this, I gauged the mortality assessment for myself to be far less than the 1 in 2000 CDC statistic.
I did not think the short-term risk of COVID was sufficient to justify the potential long-term risks from the COVID vaccines. Despite getting sick, I now have immunity to the virus, and I believe I made the right decision for myself. Of course, you might calculate differently for yourself. I believe it is a person’s right to decide whether or not the COVID vaccine is right for them.
The Case for Effective COVID Early Treatments
Having gone through COVID-19, I can say that I have more sympathy for others that have gone through it, especially for those who ended up with severe COVID and subsequently had to be transferred to the hospital.
I considered myself lucky to have been researching COVID-19 since the start of the pandemic. I was familiar with early treatment protocols, and I had the requisite supplements on hand. But what about others? Why isn’t this knowledge more widely known? There is a real need for research into early treatments and guidance for those who get sick.
Sadly, this guidance has been lacking from public health authorities. For example, during the pandemic height in 2020, too often, people who tested positive for COVID-19 were just left with the guidance “go home and, if you get worse, then go to the hospital.”
This lack of guidance did a tremendous disservice to the public, especially since there were front-line doctors, like FLCCC and America’s Frontline Doctors, who were at the forefront of pioneering treatments.
In testimony to the Texas Senate Health and Human Services Committee, Dr. Peter McCullough, professor of medicine at Texas A&M, calls the blatant disregard for COVID treatments a complete failure on the part of public health and medicine.
Dr. McCullough stated: “You get handed a diagnostic test that says ‘here you’re COVD positive – go home.’ Is there any treatment? No. Are there any resources I can call? No. Any referral lines or research hotlines? No. That’s the standard of care in the United States. How many of you have ever gotten a single word about what to do when you get handed a diagnosis? No wonder this is a complete and total failure at every level.”
It is unfortunate that public health authorities have deemphasized COVID early treatments in order to push the COVID vaccines. Public ignorance about early treatments helps with that goal but at a tremendous cost – it is hurting, even killing, Americans. So it is clear that medicine has some soul-searching to do.
It is now clear that the vaccine does not stop COVID variants, and there are currently over 100,000 reported “breakthrough” cases of COVID in fully vaccinated individuals. And, according to vaccinologist Dr. Geert Vanden Bossche, it is possibly the vaccination campaign during an ongoing pandemic that is driving the variants.
With vaccination unlikely to stop COVID-19, it is time for medicine and public health to place more of its focus on early treatments and the prevention of hospitalizations in the first place.
At this time, the CDC estimates 1 in 3 Americans have already been infected with COVID-19. That means approximately 114 million have already recovered from it. Furthermore, a new study shows that long-term immunity among those that have recovered is robust.
It will not be the vaccine that controls the pandemic but natural herd immunity obtained through COVID-19 recoveries. So let us make sure all doctors and clinicians know about early treatments so we can save lives and make that transition as smooth as possible.
By Nate Doromal